Sweet Expectations: Managing Gestational Diabetes & Preterm Risk

Pregnancy is a beautiful journey, but it can come with its share of challenges. One common concern during pregnancy is gestational diabetes mellitus (GDM). It is the most common metabolic disease & affects at least 14.7% of pregnancies globally.1 In the United States, approximately 3% to 8% of all pregnancies are diagnosed with GDM.2
What is Gestational Diabetes Mellitus (GDM)?
Gestational diabetes is a type of diabetes that develops during pregnancy. This occurs because hormones produced by the placenta can interfere with insulin function, leading to a condition known as insulin resistance. As a result, glucose accumulates in the bloodstream instead of being absorbed by the body’s cells for energy.2 GDM usually develops in the second or third trimester and often resolves after childbirth, however, it can pose risks for both the mother and baby if not managed properly.
Risk factors for Gestational Diabetes Mellitus (GDM)
While any pregnant woman can develop gestational diabetes mellitus (GDM), several factors can increase the risk. These include:
- Age (25 Years and Older): Women over 25 years old have increased risk of developing GDM.2
- Overweight or Obesity: Women with a higher body mass index (BMI) before pregnancy have an increased risk of insulin resistance, making it more difficult for the body to regulate blood sugar levels.
- Family History of Diabetes: A family history of type 2 diabetes in first-degree relatives (parents or siblings) suggests a genetic predisposition to insulin resistance and impaired glucose metabolism.
- Prediabetes (Impaired Glucose Tolerance): Women with prediabetes, a condition where blood sugar levels are higher than normal but not yet classified as diabetes, are at increased risk of developing GDM.
- Previous Pregnancy with Gestational Diabetes. 3
- Previous Pregnancy with a Large Baby: Women who have previously given birth to a baby weighing more than 9 pounds (4 kg) are at greater risk.2
- Polycystic Ovary Syndrome (PCOS): Women with PCOS, a hormonal disorder characterized by irregular menstrual cycles, excess androgen levels, and ovarian cysts have an increased risk to develop GDM.3
- Racial and Ethnic Background: Individuals from certain racial and ethnic groups, including African American, American Indian, Asian American, Hispanic or Latino, and Pacific Islander populations, have a higher prevalence of GDM.3
Understanding the risk factors for gestational diabetes mellitus (GDM) is crucial, as this condition not only impacts maternal health but also raises the likelihood of pregnancy complications, including preterm birth. Women with GDM are at a significantly increased risk of preterm birth.4 Let’s explore the connection between GDM and preterm birth, and the key factors that contribute to this increased risk.
Why Does GDM Increase the Risk of Preterm Birth?
- Poor Glycemic Control: When blood sugar levels are too high, it can lead to complications like fetal distress, where the baby isn’t getting enough oxygen or nutrients. In such cases, doctors may need to deliver the baby early via an emergency C-section to protect both the mother and the baby.5
- Polyhydramnios: A condition where there’s an excess of amniotic fluid in the uterus. Studies show that 78% of women with GDM who delivered prematurely had polyhydramnios.5 This occurs because of:
- Pressure on the Cervix: Excess fluid can put pressure on the cervix, causing it to dilate prematurely and triggering early labor.
- Abnormal fetal positioning: Polyhydramnios can also lead to abnormal fetal positioning (like breech presentation), making vaginal delivery more difficult and increasing the likelihood of a C-section.
- Hypertensive Disorders: Women with GDM are also more likely to develop hypertensive disorders during pregnancy, such as gestational hypertension or preeclampsia. These conditions can:
- Restrict Blood Flow: High blood pressure can reduce blood flow to the placenta, affecting the baby’s growth and development.
- Trigger Early Delivery: In severe cases, doctors may need to deliver the baby early to prevent life-threatening complications for the mother.
- Fetal Macrosomia: The baby grows larger than average. This can lead to:
- Difficult Vaginal Delivery: A larger baby may not fit through the birth canal, increasing the chances of a C-section.
- Birth Injuries: Macrosomia can also raise the risk of birth injuries, such as shoulder dystocia, where the baby’s shoulders get stuck during delivery.
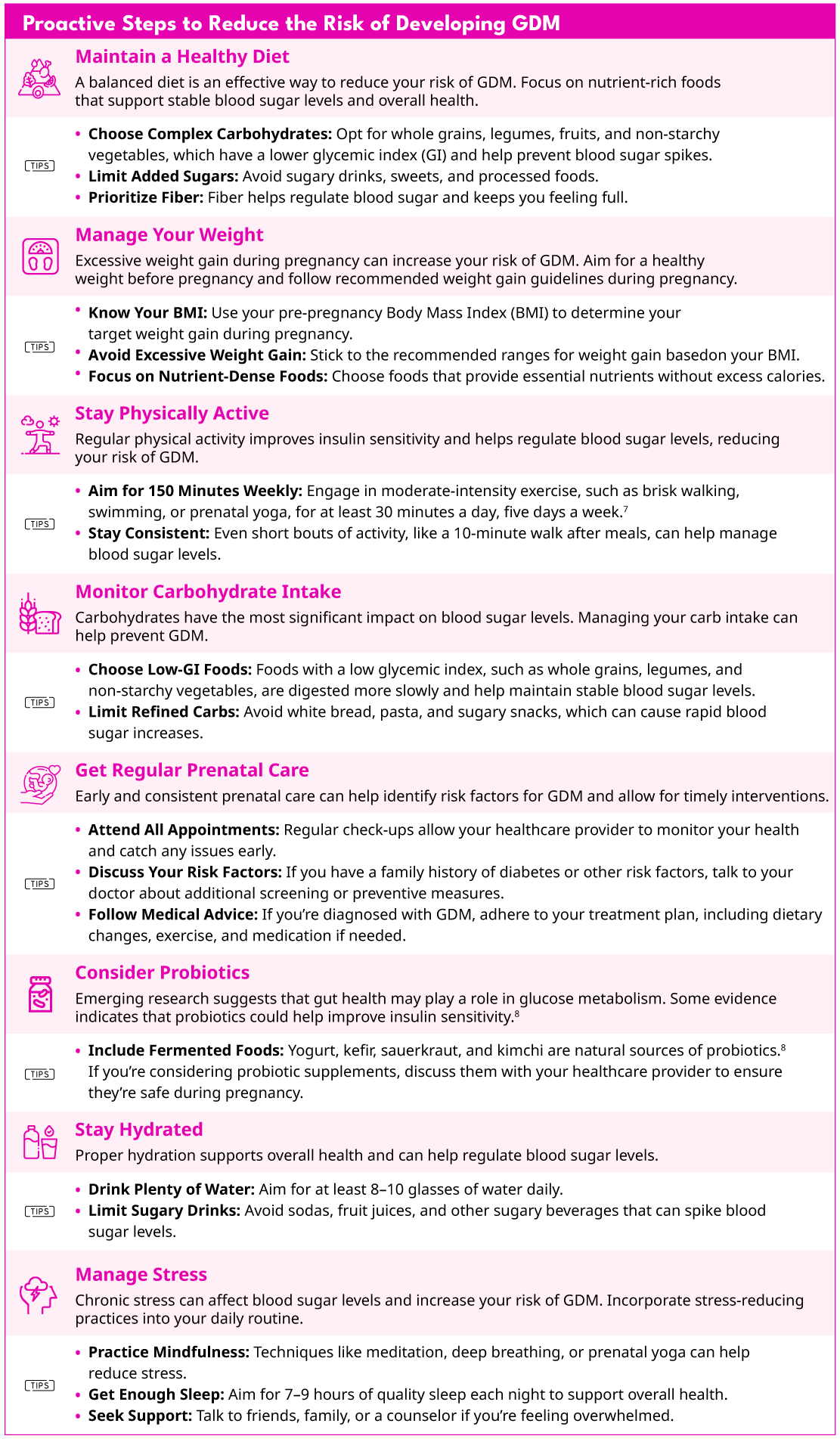
Now that we understand the risk factors, there are proactive steps you can take to reduce your risk of developing GDM. Here’s how you can make a difference:
Gestational diabetes can be a challenging diagnosis, but with the right approach, it is manageable. Each pregnancy is different, and being well-informed allows you to make the best decisions for both your health and your baby’s well-being. If you have concerns about gestational diabetes, talk to your healthcare provider about personalized strategies to manage your risk. The preemie time is wishing you health, happiness, and sweet expectations ahead! 🍯
REFERENCES
- Saeedi, M., Cao, Y., Fadl, H., Gustafson, H., & Simmons, D. (2021). Increasing prevalence of gestational diabetes mellitus when implementing the IADPSG criteria: A systematic review and meta-analysis. Diabetes research and clinical practice, 172, 108642. https://doi.org/10.1016/j.diabres.2020.108642
- Johns Hopkins Medicine. (n.d.). Gestational diabetes mellitus (GDM). Johns Hopkins Medicine. Retrieved February 7, 2025, from https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/gestational-diabetes
- https://www.cdc.gov/diabetes/about/gestational-diabetes.html
- Boriboonhirunsarn, D., & Tanpong, S. (2023). Rate of Spontaneous Preterm Delivery Between Pregnant Women With and Without Gestational Diabetes. Cureus, 15(2), e34565. https://doi.org/10.7759/cureus.34565
- Preda, A., Iliescu, D. G., Comănescu, A., Zorilă, G. L., Vladu, I. M., Forțofoiu, M. C., Țenea-Cojan, T. S., Preda, S. D., Diaconu, I. D., Moța, E., Gheorghe, I. O., & Moța, M. (2023). Gestational Diabetes and Preterm Birth: What Do We Know? Our Experience and Mini-Review of the Literature. Journal of clinical medicine, 12(14), 4572. https://doi.org/10.3390/jcm12144572
- Rasmussen, L., Poulsen, C. W., Kampmann, U., Smedegaard, S. B., Ovesen, P. G., & Fuglsang, J. (2020). Diet and Healthy Lifestyle in the Management of Gestational Diabetes Mellitus. Nutrients, 12(10), 3050. https://doi.org/10.3390/nu12103050
- Centers for Disease Control and Prevention. (n.d.). Physical activity recommendations for pregnant and postpartum women. U.S. Department of Health & Human Services. https://www.cdc.gov/physicalactivity/basics/pdfs/pa-pregnant-and-postpartum-women-508.pdf
- Mahdizade Ari, M., Teymouri, S., Fazlalian, T., Asadollahi, P., Afifirad, R., Sabaghan, M., Valizadeh, F., Ghanavati, R., & Darbandi, A. (2022). The effect of probiotics on gestational diabetes and its complications in pregnant mother and newborn: A systematic review and meta-analysis during 2010-2020. Journal of clinical laboratory analysis, 36(4), e24326. https://doi.org/10.1002/jcla.24326

Leave a Reply
Want to join the discussion?Feel free to contribute!